Abstract

SAMD9 and SAMD9L (SAMD9/9L) syndromes are new bone marrow failure (BMF) disorders with multisystem involvement (neurological, endocrine, urogenital, and others) and a propensity to develop myelodysplasia (MDS) with monosomy 7 (-7). The SAMD9/9L genes are located on chromosome 7q and are implicated in antiviral immunity, cellular growth, and protein translation. Since the discovery of germline SAMD9L mutations (SAMD9Lmut) in patients with ataxia-pancytopenia and SAMD9 mutations (SAMD9mut) in MIRAGE syndrome, several reports expanded the clinical spectrum to non-syndromic familial MDS, CANDLE syndrome, B-cell aplasia, and steroid-resistant nephrotic syndrome. Because SAMD9/9Lmut proteins enhance the growth-inhibitory effect of wildtype proteins, they are considered gain-of-function (GOF). Clonal rescue hematopoiesis is common: loss or inactivation of the mutant allele occurs by developing -7 clones, via compensatory somatic SAMD9/9Lmut, or uniparental isodisomy 7q (UPD7q). Major challenges for variant interpretation are: i) most germline mutations are novel, ii) ~70% of the mutations are classified as variants of uncertain significance (VUS), iii) the expressivity and penetrance are variable, iv) the associated phenotypes are still emerging (Sahoo, Nat Med 2021). To address these obstacles, we established a comprehensive database of SAMD9/9L variants with detailed phenotype ascertainment. We accumulated reports of SAMD9/9Lmut from literature until July 2022 (n=223) and unpublished cases in our registries (n=83). We extracted patient phenotypes, categorized them anatomically and physiologically, and evaluated correlation with genotypes and somatic events. Germline mutations were mapped using ProteinPaint (Fig 1).
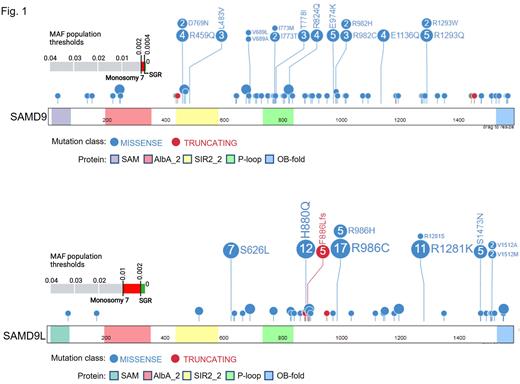
Genotypes: We assessed 306 cases with 187 unique SAMD9/9Lmut. For SAMD9 genotype 161 patients carried 122 unique germline mutations with R1293 (n=7), R982 (n=6), and E974 (n=6) discerned as frequently mutated amino acid (aa) positions. In comparison, for SAMD9L genotype, 145 SAMD9L patients had 65 unique mutations, and 3 aa residues were recurrently affected in one-third of the patients: R986 (n=22), R1281 (n=12), and H880 (n=12). Phenotypes and clinical status: Hematological abnormalities were described in 92.5% (149/161) of SAMD9mut and 83% (121/145) of SAMD9Lmut cases. The leading non-hematologic phenotypes for SAMD9mut were genitourinary (47.6%, 51/107), endocrine (36.4%, 39/107), gastrointestinal (35.5%, 38/107), neurological (20.5%, 22/107), and cardiac (11.2%, 12/107); in SAMD9Lmut patients, neurological abnormalities were predominant and found in 36% (42/116) of patients, followed by immunological abnormalities (15.5%, 18/116), while typical MIRAGE phenotypes were also observed (n=2). Within published SAMD9mut or SAMD9Lmut cases, 53% (52/98) or 75.0% (87/116) were alive at last follow-up, respectively. Of note, 63% (29/46) of the deceased SAMD9mut patients had full MIRAGE syndrome spectrum. Clonal rescue hematopoiesis: Somatic genetic rescue (SGR) with UPD7q was reported in 11.7% (26/223) of patients (SAMD9mut 5.6%; SAMD9Lmut 17.2%), SGR with somatic SAMD9/9Lmut in 22.0% (49/223) of cases (SAMD9mut 17.8%; SAMD9Lmut 25.9%), while -7 clones were present in 46.6% (104/223) of the cohort (SAMD9mut 50.5%; SAMD9Lmut 43.1%). UPD7q was more frequent in SAMD9Lmut compared to SAMD9mut (p<0.01). Moreover, 60% (24/41) of SAMD9Lmut cases with SGR (UPD7q and somatic SAMD9/9Lmut) were associated with germline mutations affecting only 4 aa residues (H880, R986, R1281, and V1512).
Lastly, we defined the population minor allelic frequency (MAF) thresholds for germline mutations based on the presence of -7 clones and adaptive SGR. We found that specific MAF thresholds were lower than the generic 0.1% and gene-specific: for -7 vs SGR in SAMD9 (0.002 vs 0.0004)and SAMD9L(0.01 vs 0.002) (Fig. 1).
Our study (www.stjude.org/samd9) represents the first effort to develop a genotype-phenotype database of SAMD9/9L syndromes which will allow investigators to deposit variants and compare them with published and unpublished data. In newly discovered predisposition syndromes, databases like the one presented here, will be instrumental in gathering crucial clinical data for variant interpretation, identify new phenotypic and prognostic correlates, and improving patients’ clinical care.
Disclosures
Erlacher:Gilead Sciences: Research Funding. Niemeyer:BMS: Honoraria; Novartis: Honoraria; Apriligen LLC: Honoraria.
Author notes
 This icon denotes a clinically relevant abstract
This icon denotes a clinically relevant abstract
Asterisk with author names denotes non-ASH members.